Evidence Based

[medical_disclaimer title=”Medical Disclaimer”]The medicines listed on this website are only there to give you knowledge. Just because they are on the list doesn’t mean that anyone will be given them; in the end, treatment decisions are up to the healthcare workers. The medicines on this list are not all of them. Doctors may recommend other drugs, even ones that don’t contain stimulants, depending on the patient’s specific health needs and circumstances.[/medical_disclaimer]
Some individuals believe that having an intense need for organization and worrying excessively about neatness is all that obsessive-compulsive disorder (OCD) is about. However, this is a common misconception, and the reality is that the illness is more complex.
OCD symptoms are defined by the Diagnostic and Statistical Manual of Mental Disorders as the presence of intrusive thoughts that are recurring and persistent, or obsessions, together with repeated, compulsive rituals performed in reaction to these ideas. Both compulsions and obsessions take a lot of time and cause severe discomfort or suffering.
Nonetheless, there are several approaches to treating OCD and improving symptom management. These approaches often work in tandem with medicine, psychotherapy, and lifestyle modifications. Continue reading to learn more about them.
Talk therapy, often known as psychotherapy, is one of the most popular treatments for obsessive-compulsive disorders. It offers a safe, accepting environment for discussing and exploring ideas, feelings, and actions. You may acquire coping mechanisms from a psychotherapist or psychologist, who can also assist you in becoming more aware of your obsessions and compulsive behaviors.
Three primary forms of psychotherapy are effective in treating OCD: acceptance and commitment therapy, exposure and response prevention therapy, and cognitive-behavioral therapy. Let’s take a closer look at them.
Due to its efficacy, cognitive-behavioral therapy (CBT) is often used as the first line of treatment for OCD and has received much investigation. Its primary objective is to assist OCD sufferers in determining what, in their specific situation, can set off obsessions and compulsions. This kind of therapy’s techniques may assist in coping with intrusive, recurrent thoughts and help replace obsessive patterns with more constructive coping methods. As a consequence, patients are able to better understand and control the relationship between the trigger and obsessive-compulsive behaviors.
In essence, exposure and response prevention treatment (ERP) is a sophisticated variation of CBT. Its primary objective is to help patients face their obsessions or anxieties without overreacting, as the name suggests.
During sessions, we gradually expose patients to ideas, pictures, objects, or circumstances that cause them to become fixated. They also engage in certain activities that, without the need for rituals, help them handle stress and anxiety. This approach gradually breaks the loop of obsessions and compulsions.
The mindfulness-based method of acceptance and commitment therapy (ACT) is used. Rather than attempting to ignore or control painful thoughts and sensations, it might assist people in accepting them.
When using ACT to treat OCD, the primary objective is to help the patient accept their thoughts and obsessions and encourage behaviors that are motivated by values. ACT primarily aids in enhancing psychological adaptability and lessening the impact of the illness on day-to-day experiences.
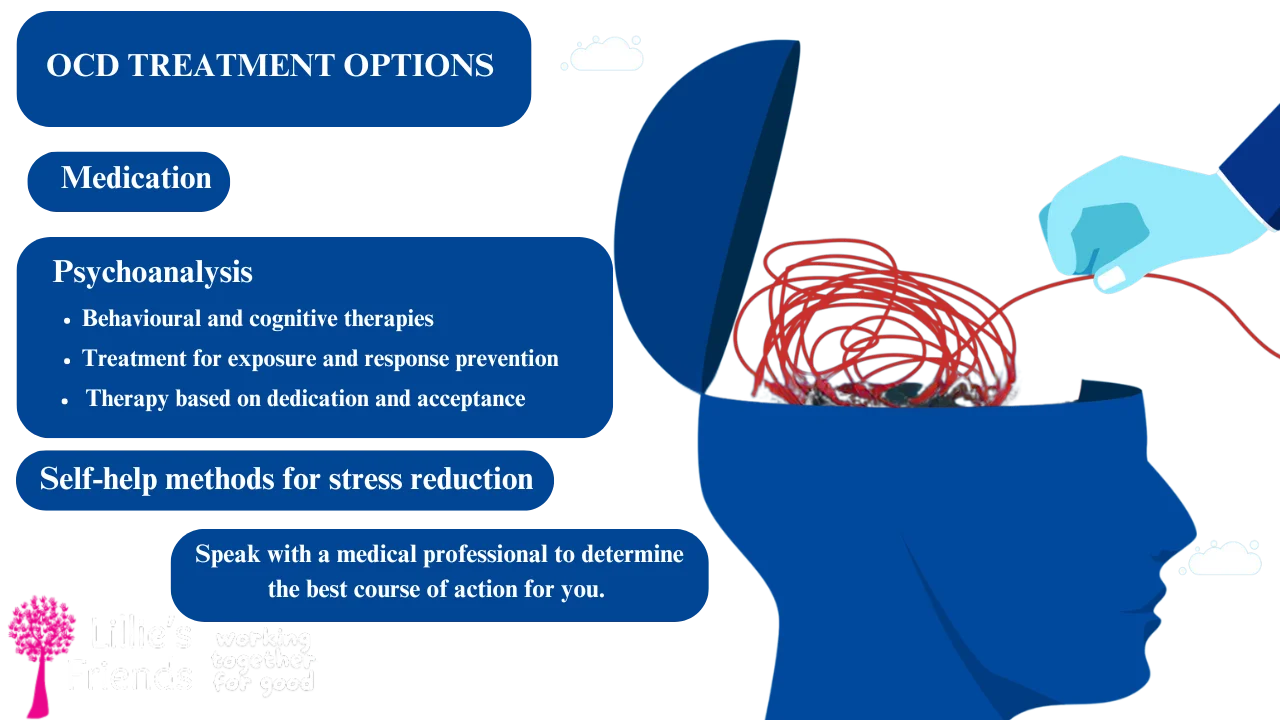
Medication is frequently considered when OCD symptoms range from mild to severe and psychotherapy doesn’t seem to be working well enough. The following are the most often recommended drugs for the treatment of OCD:
There are several OCD therapies available, so it’s critical to choose the one that best meets your requirements. The degree of symptoms, responsiveness to prior therapies, coexisting diseases, and possible side effects all play a role in the decision of which drug to take. Finding the right drug and dose requires discussing every element of your medical history with a healthcare professional.
The drugs recommended for OCD may have negative effects, just like any other treatments. Some are common and mild, going away with time, while others may be more serious, necessitating stopping the medicine and selecting an alternative.
Agitation, anxiety, nausea, constipation, diarrhea, migraines, and sleeplessness are among side effects of SSRIs. Compared to SSRIs, clomipramine has a greater frequency of adverse effects, therefore taking it needs additional care. Dry mouth, constipation, weight gain, drowsiness, impaired vision, and low blood pressure are typical side effects. Atypical antipsychotics may also have adverse effects that include mood swings, sleepiness, changes in weight, and sexual dysfunction.
To prevent side effects, it’s essential to adhere strictly to the prescribed course of therapy for OCD. Additionally, don’t forget to let your healthcare physician know about any worries or adverse effects. Finding a remedy that offers more advantages than disadvantages would be beneficial.
Drugs may interact with over-the-counter vitamins, certain foods, and other medications.
Apart from the conventional therapy modalities mentioned before, your healthcare professional could suggest other possibilities. If you have a severe type of OCD and don’t react well to the recommended courses of therapy or just want to ensure that your treatment plan is working, then it can be a wise choice.
Those suffering from OCD may need support from those facing the same difficulties, even when they get the best therapy available. According to studies, support groups are a useful resource for OCD sufferers since members may exchange beneficial self-help techniques and discuss their experiences. Support groups can help you avoid anxiety, reduce loneliness, and create a social environment that is encouraging.
Stress may sometimes worsen OCD symptoms, making it more challenging to manage worries and intrusive thoughts. Thus, maintaining healthy habits and implementing additional stress-reduction strategies into everyday life might be beneficial:
Treatment-resistant patients and those with severe OCD may benefit from deep brain stimulation (DBS) . Despite being relatively new and uncommon, this approach has shown a significant improvement in symptoms. During DBS, doctors surgically place electrical conductors in certain brain areas, like the prefrontal-subcortical circuits, that are connected to OCD symptoms.
The FDA has aauthorizedtranscranial magnetic stimulation (TMS) for the treatment of major depressive disorders and obsessive-compulsive disorders. This non-invasive process creates a magnetic field that travels through the skull and activates areas of the brain underneath it. It may assist in modifying the brain circuits that OCD has created and alleviate its symptoms.
A thorough treatment strategy is necessary for OCD, which may include a mix of techniques. While some individuals may benefit from medication or a mix of many approaches, others may benefit more from counseling.

For those with minor symptoms, or as a supplement to psychotherapy and medication, self-help strategies may be beneficial. It is advisable to seek therapy for OCD from a qualified healthcare provider since they are capable of developing a customised, all-encompassing strategy that addresses even the most minor symptoms.

Each person’s odds of fully recovering from OCD vary. While some people may have much better symptoms, others can have a more enduring ailment. It’s critical to understand that total healing does not include the elimination of all obsessive thoughts. It is figuring out how to control and minimise the influence of these ideas on day-to-day existence. Also take notice of the fact that good treatment outcomes are usually increased with early diagnosis

Untreated OCD may cause symptoms to increase to the point that they start to interfere with day-to-day activities, such as relationships and employment. It may also raise the likelihood of drug misuse and suicidal thoughts, as well as lead to the emergence of further mental health issues, including depression and anxiety disorders.

Even the best therapies aren’t always able to totally eradicate intrusive thoughts and compulsions. However, the majority of the time, drugs, counselling, and complementary therapies greatly reduce symptoms. Long-term professional therapy may also teach you helpful coping mechanisms and self-help techniques to handle OCD symptoms at any time.